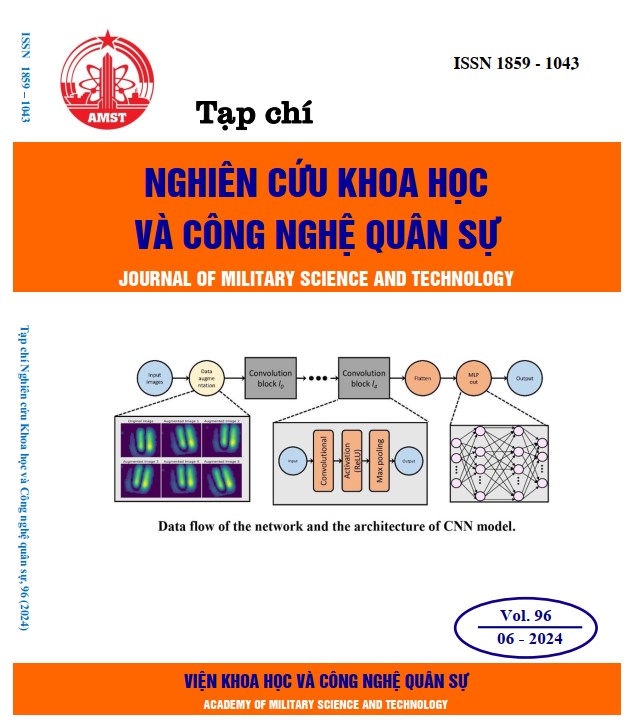
Development of a passive wireless sensor for fluidic detection and characterization utilizing the PCB-based coplanar electrode (PCE) configuration
371 viewsDOI:
https://doi.org/10.54939/1859-1043.j.mst.96.2024.116-123Keywords:
Fluidic detection; LC passive wireless sensing; Printed circuit board; Glucose biosensors.Abstract
During the global economic development, there's a growing focus on healthcare, especially in the advancement of medical diagnostic technologies, with a significant emphasis on glucose level evaluation. Glucose biosensors, predominantly electrochemical, have evolved over four generations, with the first three being enzyme-based and known for sensitivity and cost-effectiveness, albeit with limitations due to environmental susceptibility and reliance on enzyme activity. Recent advancements in non-invasive blood glucose monitoring, utilizing optical, microwave, and electrochemical techniques, offer diverse benefits without tissue penetration. Among these, impedance sensing stands out due to its flexibility and integration capability in handheld devices. This study proposes a wireless passive impedance method leveraging the inductor-capacitor (LC) sensing technique and PCB (Printed Circuit Board)-based coplanar electrode (PCE) configuration for fluidic sample detection. The proposed system integrates a two-coplanar-electrode layout with a square spiral inductor to assess fluidic conductivity and characterize various fluid types within samples. The effectiveness of this configuration was validated through experiments with NaCl and glucose solutions, confirming the feasibility of integrating PCB-based coplanar electrodes into conventional LC passive wireless sensing designs for fluidic detection and characterization.
References
[1]. Weibel M K and H J Bright, “The glucose oxidase mechanism. Interpretation of the pH dependence” The Journal of biological chemistry, vol. 246, no. 9, pp. 2734–44, (1971), [Online]. Available: http://www.ncbi.nlm.nih.gov/pubmed/4324339 DOI: https://doi.org/10.1016/S0021-9258(18)62246-X
[2]. Yoo Eun-Hyung and Soo-Youn Lee, “Glucose Biosensors: An Overview of Use in Clinical Practice,” Sensors, vol. 10, no. 5, pp. 4558–4576, (2010), doi: 10.3390/s100504558. DOI: https://doi.org/10.3390/s100504558
[3]. Balas Costas, “Review of biomedical optical imaging—a powerful, non-invasive, non-ionizing technology for improving in vivo diagnosis,” Measurement Science and Technology, vol. 20, no. 10, p. 104020, (2009), doi: 10.1088/0957-0233/20/10/104020. DOI: https://doi.org/10.1088/0957-0233/20/10/104020
[4]. Walther Julia, Maria Gaertner, Peter Cimalla, Anke Burkhardt, Lars Kirsten, Sven Meissner, and Edmund Koch, “Optical coherence tomography in biomedical research,” Analytical and Bioanalytical Chemistry, vol. 400, no. 9, pp. 2721–2743, (2011), doi: 10.1007/s00216-011-5052-x. DOI: https://doi.org/10.1007/s00216-011-5052-x
[5]. Boppart Stephen A., Amy L. Oldenburg, Chenyang Xu, and Daniel L. Marks, “Optical probes and techniques for molecular contrast enhancement in coherence imaging,” Journal of Biomedical Optics, vol. 10, no. 4, p. 041208, (2005), doi: 10.1117/1.2008974. DOI: https://doi.org/10.1117/1.2008974
[6]. Kollias Nikiforos and Georgios N. Stamatas, “Optical Non-Invasive Approaches to Diagnosis of Skin Diseases,” Journal of Investigative Dermatology Symposium Proceedings, vol. 7, no. 1, pp. 64–75, (2002), doi: 10.1046/j.1523-1747.2002.19635.x. DOI: https://doi.org/10.1046/j.1523-1747.2002.19635.x
[7]. Naikoo Gowhar A., Hiba Salim, Israr U. Hassan, Tasbiha Awan, Fareeha Arshad, Mona Z. Pedram, Waqar Ahmed, and Ahsanulhaq Qurashi, “Recent Advances in Non-Enzymatic Glucose Sensors Based on Metal and Metal Oxide Nanostructures for Diabetes Management- A Review,” Frontiers in Chemistry, vol. 9, (2021), doi: 10.3389/fchem.2021.748957. DOI: https://doi.org/10.3389/fchem.2021.748957
[8]. Li Hong, Haibo Xu, Shiru Lin, and Yi Jia, “A Wireless Resonant LC Sensor for Glucose Detection,” in The 9th International Electronic Conference on Sensors and Applications, (2022), p. 29. doi: 10.3390/ecsa-9-13365. DOI: https://doi.org/10.3390/ecsa-9-13365
[9]. Jang Chorom, Hee-Jo Lee, and Jong-Gwan Yook, “Radio-Frequency Biosensors for Real-Time and Continuous Glucose Detection,” Sensors, vol. 21, no. 5, p. 1843, (2021), doi: 10.3390/s21051843. DOI: https://doi.org/10.3390/s21051843
[10]. Li Yang, Zhao Yao, Wenjing Yue, Chunwei Zhang, Song Gao, and Cong Wang, “Reusable, Non-Invasive, and Ultrafast Radio Frequency Biosensor Based on Optimized Integrated Passive Device Fabrication Process for Quantitative Detection of Glucose Levels,” Sensors, vol. 20, no. 6, p. 1565, (2020), doi: 10.3390/s20061565. DOI: https://doi.org/10.3390/s20061565
[11]. Zafar Hima, Asma Channa, Varun Jeoti, and Goran M. Stojanović, “Comprehensive Review on Wearable Sweat-Glucose Sensors for Continuous Glucose Monitoring,” Sensors, vol. 22, no. 2, p. 638, (2022), doi: 10.3390/s22020638. DOI: https://doi.org/10.3390/s22020638
[12]. Dautta Manik, Muhannad Alshetaiwi, Jens Escobar, and Peter Tseng, “Passive and wireless, implantable glucose sensing with phenylboronic acid hydrogel-interlayer RF resonators,” Biosensors and Bioelectronics, vol. 151, p. 112004, (2020), doi: 10.1016/j.bios.2020.112004. DOI: https://doi.org/10.1016/j.bios.2020.112004
[13]. Moschou Despina and Angeliki Tserepi, “The lab-on-PCB approach: tackling the μTAS commercial upscaling bottleneck,” Lab on a Chip, vol. 17, no. 8, pp. 1388–1405, (2017), doi: 10.1039/c7lc00121e. DOI: https://doi.org/10.1039/C7LC00121E
[14]. Kontakis Konstatinos, Anastasios Petropoulos, Grigoris Kaltsas, Thanassis Speliotis, and Evangelos Gogolides, “A novel microfluidic integration technology for PCB-based devices: Application to microflow sensing,” Microelectronic Engineering, vol. 86, no. 4–6, pp. 1382–1384, (2009), doi: 10.1016/j.mee.2009.01.088. DOI: https://doi.org/10.1016/j.mee.2009.01.088
[15]. Liu Robin Hui, Piotr Grodzinski, Jianing Yang, and Ralf Lenigk, “Self-Contained, Fully Integrated Biochips for Sample Preparation, PCR Amplification and DNA Microarray Analysis,” Integrated Biochips for DNA Analysis, vol. 76, no. 7, pp. 46–67, (2008), doi: 10.1007/978-0-387-76759-8_4. DOI: https://doi.org/10.1007/978-0-387-76759-8_4
[16]. Sánchez J. L.Acero, O. Y.F. Henry, H. Joda, B. Werne Solnestam, L. Kvastad, E. Johansson, P. Akan, J. Lundeberg, N. Lladach, D. Ramakrishnan, I. Riley, and C. K. O’Sullivan, “Multiplex PCB-based electrochemical detection of cancer biomarkers using MLPA-barcode approach,” Biosensors and Bioelectronics, vol. 82, pp. 224–232, (2016), doi: 10.1016/j.bios.2016.04.018. DOI: https://doi.org/10.1016/j.bios.2016.04.018
[17]. M. Lewis A, L. L. Wu, S. Babikian, M. Bachman, J. G Santiago, “SI: An Integrated Printed Circuit Board Device for Cell Lysis and Nucleic Acid Extraction S-1 S-4 Temperature-induced pressure S-2 S-3 Experimental Rayleigh num-,” Analytical Chemistry, pp. 1–7, (2012).
[18]. Do Quang Loc, Tung Thanh Bui, Anh Bao Hoang, Pham Van Thanh, Chun Ping Jen, and Trinh Chu Duc, “Development of a Passive Capacitively Coupled Contactless Conductivity Detection (PC4D) Sensor System for Fluidic Channel Analysis Toward Point-of-Care Applications,” IEEE Sensors Journal, vol. 19, no. 15, pp. 6371–6380, (2019), doi: 10.1109/JSEN.2019.2908179. DOI: https://doi.org/10.1109/JSEN.2019.2908179
[19]. Miao Fengjuan, Hao Wu, Bairui Tao, and Yu Zang, “A passive-chipless LC carbon dioxide sensor with non-contact ZnO/CuO/RGO nanocomposites at room temperature,” Vacuum, vol. 215, p. 112261, (2023), doi: 10.1016/j.vacuum.2023.112261. DOI: https://doi.org/10.1016/j.vacuum.2023.112261
[20]. He Denghui, Yuanhui Cui, Fangchao Ming, and Weiping Wu, “Advancements in Passive Wireless Sensors, Materials, Devices, and Applications,” Sensors, vol. 23, no. 19, p. 8200, (2023), doi: 10.3390/s23198200. DOI: https://doi.org/10.3390/s23198200